Eye Conditions
Astigmatism
One of the four major refractive errors is Astigmatism
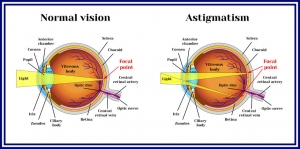
Refractive errors of the eye occur when the image does not focus on the retina at the back of the eye, causing blurred vision. In Astigmatism when light enters the eye instead of focusing on the retina at the back of the eye it splits and focuses in two different places.
.
This causes different amounts of blur in different directions, so images appear distorted and vision is usually blurred at all distances. Even small amounts of Astigmatism can cause symptoms such as headaches, fatigue and problems especially when concentrating, as the eyes try without success to correct the blur and distortion.
Astigmatism is an inherited characteristic but can also be a normal variation of development; it is not an eye disease, with most people having at least some degree of Astigmatism. It is usually caused by uneven curvature of the cornea (the front surface of the eye) being different in different meridians, like an Australian football in shape instead of a soccer ball. In other cases the Astigmatism can be due to the lens inside the eye being tilted.
Astigmatism is classified as regular or irregular, in regular Astigmatism, the principal meridians are 90 degrees apart or perpendicular to each other, whereas in irregular Astigmatism, the principal meridians are not perpendicular. Most Astigmatism is regular and can be Myopic (short sighted), Hyperopic (long sighted) or Mixed (Hyperopic and Myopic). Irregular Astigmatism can result from corneal scarring due to injuries, some types of eye surgery or certain diseases of the cornea such as Keratoconus.
Astigmatism can be corrected by both spectacles and contact lenses; sometimes correction of Astigmatism can initially cause a change in the apparent size and shape of objects and this may affect depth perception. In some cases it can take time for the brain to adjust to new spectacles when correcting Astigmatism with objects appearing sloped or curved, this usually settles down with wear. In most cases, adjustment to these side effects takes only a week or so.
Cataract
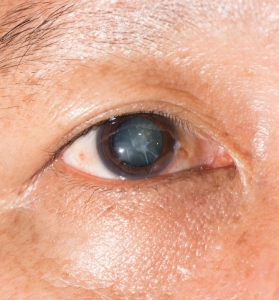
As they progress Cataracts become larger and denser causing vision to worsen over time, usually both eyes are affected but one eye is usually worse. If untreated, Cataracts can cause blindness as the lens becomes too dense to see through. People over the age of 65 often have signs of Cataracts and should have their eyes examined annually, regular eye examinations allow Cataracts to detected early, progression monitored and referral for surgery initiated when required.
Cataract surgery in the modern world is now a relatively simple day procedure, and is often performed under local anaesthetic. The surgeon removes the cloudy lens and replaces it with a new Intra-ocular lens which improves the vision; in most cases spectacles will still be necessary at least for reading.
Diabetes
 Diabetes is fast becoming an epidemic in the 21st century with around 1.7 million Australians suffering from the condition and these figures are on the rise with 280 new cases being diagnosed daily. Diabetes affects the entire body and although it can be well managed it has the potential for serious complications, including blindness. 70% of people suffering from Diabetes will develop some changes in their eyes within 15 years of diagnosis, and with Diabetic eye disease being the leading cause of blindness in working age adults, regular eye examinations should be a routine part of any Diabetic management plan.
Diabetes is fast becoming an epidemic in the 21st century with around 1.7 million Australians suffering from the condition and these figures are on the rise with 280 new cases being diagnosed daily. Diabetes affects the entire body and although it can be well managed it has the potential for serious complications, including blindness. 70% of people suffering from Diabetes will develop some changes in their eyes within 15 years of diagnosis, and with Diabetic eye disease being the leading cause of blindness in working age adults, regular eye examinations should be a routine part of any Diabetic management plan.
Diabetes can cause many problems within the eye, some more serious than others. Vision can fluctuate from day to day; this is often an early sign and has led to the diagnosis of Diabetes in some patients. The problem usually resolves when blood glucose levels are brought under control. In some cases double vision can be present, this is a rare complication but can be quite distressing, the double vision is usually temporary but it may take a few months to resolve. Patients with Diabetes will often develop Cataracts earlier than those who are not Diabetic, and the Cataracts tend to worsen more quickly, this is due to the changes in the blood glucose causing changes to the crystalline lens in the eye, which initially requires frequent changes to your spectacle prescription and then eventually surgery.
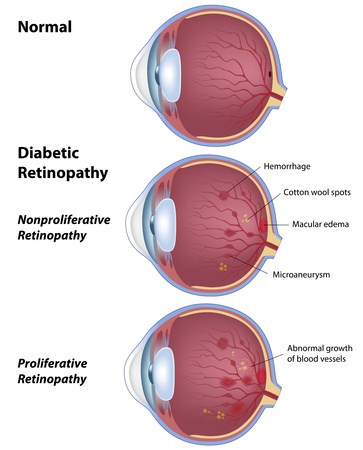
Of all the complications within the eye caused by Diabetes the most serious is Diabetic Retinopathy, this is when the high blood sugar causes damage to the blood vessels in the retina at the back of the eye. The vessels can swell and leak, they can occlude, stopping blood from passing through and in some cases abnormal new vessels can grow on the retina. The risk of developing retinopathy increases with the length of time you have had Diabetes, and those with poor control of their blood glucose levels are more at risk. Diabetic retinopathy has the potential to cause serious and irreversible vision loss, controlling blood glucose over time significantly reduces the risk of developing retinopathy, but does not eliminate it.
The best management is to have regular eye examinations so that changes can be detected and treated early. It is advisable for all people with diabetes to have yearly eye examinations, more frequently if any problems are detected. During your eye examination your pupils will be dilated, retinal photos taken and the eye examined for any changes, early detection, improved blood glucose control and early treatment are an essential part of preserving eye sight. Vision is a precious gift, so if you are Diabetic and haven’t had an eye examination in the last year then don’t delay and book an appointment with us today.
Click on logo to visit Diabetes Australia:
Dry Eye

“Dry Eye is a very common problem”
Dry Eye is a very common problem, particularly among older people and females. It is essentially a dysfunction of the tear film, with some people not producing enough tears and others having a poor quality tear film. Both result in the eye not being wet enough causing symptoms of discomfort such as irritation, stinging, burning, scratchiness, foreign body sensation, light sensitivity, stringy mucus and unstable vision between blinks.
Sometimes, a wet eye is actually a dry eye and increased tearing may actually be a symptom of dry eyes. If your tear secretions are below the normal quality or quantity, excess tears are produced by the lacrimal gland. This happens in response to the irritation caused on the surface of the eye due to the lack of moisture that your tears provide. These excess tears are below standard and not greasy enough, so where they provide initial relief they do not solve the problem of dry eyes in the long term. So even though the eyes are basically dry, sufferers can appear as if they are crying, this is worse in dry air or windy environments.
Use of certain medications like antihistamines, oral contraceptives and antidepressants, as well as general health problems like Arthritis or Sjogren’s syndrome; problems with blinking and eyelid disorders also cause problems with dry eye. Dependant on the type of dry eye and the cause of symptoms, relief can be provided by the use of Tear supplements, protection from the elements, dietary supplements, warm compresses and lid hygiene, or in some cases Manuka honey eye drops.
Glaucoma
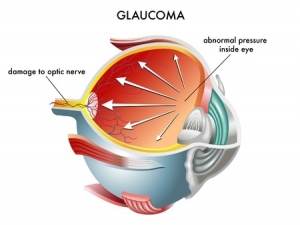 Glaucoma is a disease that causes damage to the optic nerve, the bundle of nerve fibres that carries information from the eye to the brain; optic nerve damage is usually associated with high intraocular pressure but this is not always the case. If untreated Glaucoma progressively leads to vision loss and in severe cases blindness, where only a small central section of vision is left or the person is completely blind. The longer the disease is untreated, the greater the likelihood of damage, furthermore this damage is irreversible but with appropriate treatment this damage can be stopped, this is initially in the form of drops or in more severe cases surgery.
Glaucoma is a disease that causes damage to the optic nerve, the bundle of nerve fibres that carries information from the eye to the brain; optic nerve damage is usually associated with high intraocular pressure but this is not always the case. If untreated Glaucoma progressively leads to vision loss and in severe cases blindness, where only a small central section of vision is left or the person is completely blind. The longer the disease is untreated, the greater the likelihood of damage, furthermore this damage is irreversible but with appropriate treatment this damage can be stopped, this is initially in the form of drops or in more severe cases surgery.
In its early stages Glaucoma has no symptoms and sufferers will be are unaware there is a problem until it is too late and permanent damage may have occurred. In some more acute cases the increased pressure in the eye will cause blurred vision, apparent coloured rings around lights, loss of side vision, and pain and redness of the eye.
Early detection and treatment are the best way to control Glaucoma, during an eye examination we can look at the optic nerve, measure eye pressures and also test visual fields to assess for the disease. Everyone should have regular 2 yearly eye examinations but people over the age of 40 and those with a family history of Glaucoma are more at risk.
 |
Hyperopia
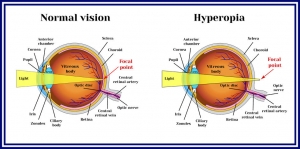
In the normal eye, when light enters the eye it is bent or refracted by the cornea so that it creates a focussed image on the retina at the back of the eye. In Hyperopia the eye is either too short or the power of the optical components not strong enough, so that light fails to come to a focus on the retina, instead focussing on a virtual spot behind the eye.
Mild Hyperopia is not usually a problem because the lens inside our eyes can compensate, but if a significant amount of Hyperopia is present, the effort to focus or accommodate can be too great. The closer the object the more accommodation is required to focus it, this effort can lead to symptoms such as eyestrain, fatigue and headaches especially when doing near work such as using the computer or reading.
Because a Hyperopic person can often see well in the distance, checking vision with a letter chart alone (such as during a school screening) may miss it. Children are usually slightly Hyperopic at a young age but become Emmetropic (normal vision) as they grow. In some cases the Hyperopia remains and may worsen causing problems with vision. When a child is young they have strong accommodation so often it is not picked up until they go to school when they may struggle with reading and close work. As we get older our accommodation reserves deplete so it becomes harder to focus so Hyperopia becomes more of a problem with age. For this reason Hyperopia is often confused with Presbyopia which affects people after 40 and is a different condition.
A comprehensive eye examination is the only way to pick up Hyperopia, it is recommended that children have a check up prior to starting school to ensure that their eyes have developed normally. Anyone experiencing headaches, eyestrain or fatigue should also have their eyes checked as the culprit may be Hyperopia. Call us today to book an appointment.
Keratoconus
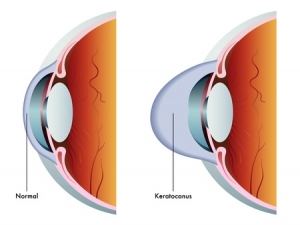
Keratoconus is a disorder of the Cornea on the anterior surface of the eye, where the cornea thins causing it to bulge from its normal round shape to a cone shape, distorting vision. It is a progressive disorder but the speed of change is unpredictable, generally the condition progresses slowly and can cease at any stage. While Keratoconus interferes with visual clarity it rarely causes blindness.
In the early stages, Keratoconus causes slight blurring and distortion of vision, increased sensitivity to glare and light and can be corrected with spectacles but as the condition progresses, good vision cannot be achieved with glasses. The use of specialised rigid contact lenses is often the best method of correcting vision, and most people successfully manage Keratoconus in this way. However in a small number of more advanced cases, a corneal transplant may be needed, although newer treatment options like Collagen X linking and Intra-stromal rings are now becoming available.
For more information click on logo go to Keratoconus Australia website:
 |
Macula Degeneration
AMD is caused by ageing processes in the eye; there are two main forms wet and dry, both begin in the Retinal Pigment Epithelium (RPE), this layer of cells is responsible for passing oxygen and other essential nutrients to the retina and removing waste products. When this waste disposal system breaks down, the waste builds up and deposits form on the retina, causing distortion which can damage other layers.
AMD is the major cause of vision impairment and blindness in Australia for people over the age of 50, the wet form is the more aggressive form accounting for approximately 10-15% of cases but accounting for around 90% of all cases of severe vision loss from the disease. In wet AMD new blood vessels can grow into the Macula; these new vessels are fragile and are prone to leaking, this can lead to scar tissue, which once present severely affects vision.
In the early stages of AMD, sufferers may not realize anything is wrong and still function normally, or people may notice problems with reading even when their reading spectacles are worn. As AMD progresses, vision loss progressively worsens, there is no cure for AMD and treatment only attempts to slow this progressive loss, the earlier the disease is detected, the more vision that is likely to be retained.
It is essential to have regular eye examinations to detect the disease as early as possible, during an eye examination we can detect the presence of AMD in the early stages by taking retinal photos and looking at the Macula with a slit-lamp and a high-powered lens. An Amsler grid can also be used to look for problems; these can also be easily used at home. Regular eye examinations are particularly important for people over the age of 50, those with a family history of the condition and smokers. Research has found that reducing exposure to UV light and cigarette smoke, and eating a diet rich in green leafy vegetables, nuts and fish may be beneficial in reducing the impact of AMD.
Click on logo below to visit Macular Disease Foundation Australia
Myopia
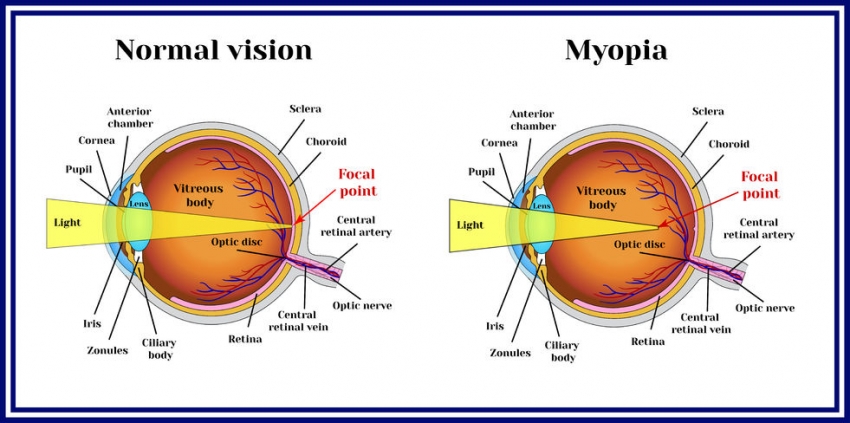
In the normal eye, when light enters the eye it is bent or refracted by the cornea so that it lands on the retina to create a focussed image. In Myopia the light focuses short of the retina creating a blurred image, this is due to either the length of the eye being too long, or the curvature of the cornea being too great.
Myopia usually develops in childhood and there is often a family history of the condition. It usually worsens throughout the teenage years before stabilising in the mid 20’s, after which there may be little or no change in vision. The onset of myopia may be slow and only change gradually, but in other cases it comes on suddenly and changes rapidly.
The first signs of Myopia in childhood often present when a child starts going to school, with difficulty reading the board, or seeing the teacher clearly. Often Myopic children will screw up their eyes, sit close to the television and lack interest in playing outdoor games.
The exact causes of myopia are not known, excessive amounts of reading; poor metabolism, poor diet, poor light, poor posture and genetic factors have all been considered. Current research indicates that the development of myopia is influenced by both genetic and environmental factors.
A comprehensive eye examination is the only way of determining whether you or your child has Myopia. Call us today to book an appointment.
Presbyopia

Having trouble seeing close up?
One of the four major refractive errors is Presbyopia, a common condition that affects close tasks such as reading, sewing and computer use. People often find that they have to hold things further away to see them more clearly. Presbyopia is a normal ageing process and will affect everyone after a certain age it cannot be prevented, but it does not affect distance vision.
Presbyopia is usually first noticed around the age of 40 to 45 years, as the ability of the eye to focus on objects at near starts to reduce, this is due to changes in the lens in the eye. When we focus on close objects, a muscle in the eye changes the shape of the lens in a process called accommodation, with increasing age the lens hardens and loses its flexibility. The loss in lens flexibility causes a decrease in the ability of the eye to accommodate, which is the reason that focusing at near becomes more difficult.
Although it may seem that difficulty with close work comes on suddenly, Presbyopia comes on gradually and is a normal ageing process and has been going on since childhood. Between the ages of 45 and 65, the amount of Presbyopia increases, making near work more and more difficult, it usually stabilises from 65 years onwards. During this time it is important to have regular 2 yearly eye tests, in some cases vision can change faster than this and more frequent check ups are required.
Presbyopia is corrected by a prescription designed especially for close work, this is different to any distance correction you may have. The correction for Presbyopia will make near objects clear but distant objects blurry, this means that single focus reading spectacles will be blurry in the distance. Luckily other options such as bifocals, trifocals or progressive lenses are available. Wearing spectacles will not speed up or slow the progression of Presbyopia as it is an ageing process, it will continue regardless of whether spectacles are worn or not, so why struggle.
The team at Eyewise Optometrists will be happy to discuss your specific requirements with you during your eye test and your spectacle dispense to ensure we come up with a solution for your needs.
Pterygium
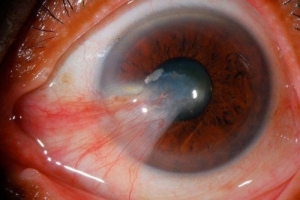 A Pterygium is a triangular shaped vascularised growth which extends from the conjunctiva (the thin membrane covering the white of the eye) onto the central cornea (the clear part of the eye over the coloured iris). There is a strong association between development of Pterygia and exposure to ultraviolet radiation and hot, dry environments. They are more common in people who live in rural environments, the north of Australia and those that spend a lot of time outdoors. Although Pterygia are not dangerous they do tend to worsen with time, causing discomfort, irritation, redness and in some cases may interfere with vision as their growth can cause the cornea to distort. For some they are also a cosmetic concern.
A Pterygium is a triangular shaped vascularised growth which extends from the conjunctiva (the thin membrane covering the white of the eye) onto the central cornea (the clear part of the eye over the coloured iris). There is a strong association between development of Pterygia and exposure to ultraviolet radiation and hot, dry environments. They are more common in people who live in rural environments, the north of Australia and those that spend a lot of time outdoors. Although Pterygia are not dangerous they do tend to worsen with time, causing discomfort, irritation, redness and in some cases may interfere with vision as their growth can cause the cornea to distort. For some they are also a cosmetic concern.
As the development of Pterygia is associated with ultraviolet light, the best way to protect your eyes from developing a Pterygium or to slow the progression of an existing one is to protect your eyes from UV. This can be done by wearing a broad brimmed hat, wrap-around sunglasses and avoiding the sun between 10 am and 3 pm when UV radiation is strongest. UV radiation can also cause cataracts, other eye diseases, as well as skin cancers, so reducing exposure has many health benefits. In some cases UV protection will often stabilize the growth of a Pterygium and provided that vision is not being affected this may be all that is required. At times though a Pterygium can cause discomfort or become inflamed, eye drops or ointments may be beneficial during these times. In some cases where a Pterygium is actively growing and threatening vision, then surgical removal is the only option.
As Pterygia are a progressive disorder and it is not uncommon for them to grow back after surgical removal a regular eye examination to monitor their progress is recommended. At Eyewise Optometrists we can take anterior segment photos enabling us to compare any changes over time.
Floaters, Spots and Flashes
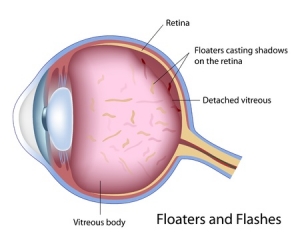 any problems. The term “Floaters” is used for spots, specks, threads, or cobweb-like images that occasionally drift across the line of sight; they can be of all sizes and shapes. Floaters form when the vitreous (the jelly which fills the eye) shrinks with age, causing it to become a bit stringy, these strands then cast shadows on the retina as they move across the line of sight. The vitreous also acts as the eye’s shock absorber so active people and those with previous injuries are more prone to developing floaters. Most people tolerate floaters with no problems but for others they affect vision as they drift past especially when reading.
any problems. The term “Floaters” is used for spots, specks, threads, or cobweb-like images that occasionally drift across the line of sight; they can be of all sizes and shapes. Floaters form when the vitreous (the jelly which fills the eye) shrinks with age, causing it to become a bit stringy, these strands then cast shadows on the retina as they move across the line of sight. The vitreous also acts as the eye’s shock absorber so active people and those with previous injuries are more prone to developing floaters. Most people tolerate floaters with no problems but for others they affect vision as they drift past especially when reading.
When floaters appear they can sometimes be associated with flashes of light or sparks in the vision, these flashes occur due to the shrinking vitreous pulling on the light sensitive retina at the back of the eye. This pulling is often associated with a Posterior Vitreous Detachment (PVD), which most of us will experience at some stage as we get older and usually does not have any serious consequences. However, in some individuals when the vitreous shrinks it can cause a hole or tear in the retina, causing a more serious Retinal Detachment (RD) which can lead to permanent vision loss.
Both a PVD and a RD are painless and present with the same symptoms of flashes and floaters, RD requires urgent referral so it is essential to have a prompt comprehensive retinal examination if you become aware of these symptoms, to rule out the presence of a retinal tear, hole or detachment. Floaters on their own in general are harmless they are not treated and will break down over time and in most cases become less noticeable.